History Taking and Examination
The diagnosis of any disease depends upon three things: History, examination and investigations. In ophthalmology. about 80% of the diseases are diagnosed by history and examination and about 20% cases need investigations. Therefore, detailed history and proper examination of an eye is important for diagnosis of most of the ocular diseases.
PROTOCOL OF EYE EXAMINATION
- History
2 Pattern of examination
Ocular examination-It includes
- Physical examination
- Functional examination
b. Systemic examination
- Methods (techniques) of examination
- Investigations
HISTORY TAKING
The pattern of history taking is similar to that in medicine and surgery such as:
- Presenting symptoms
- History of present illness
- Past history-medical and surgical history
- Family history
- Personal history Socioeconomic condition
The common presenting symptoms in ocular diseases are:
- Disturbances of vision for distance, near or both which may be gradual, sudden, painful or painless. Pain in the eye/eyestrain or headache.
- Redness of the eye
- Abnormal secretion/discharge
- Defective dark adaptation or night blindness
- Abnormal colour vision
- Halos (iridescent vision)
- Floaters
- Flashes of light
- . Photophobia
- Diplopia/polyopia
- Metamorphopsia (distorted images)
- Deviation of eyes (crossed eyes)
- Protrusion (forward displacement) of an eye
PATTERN OF EXAMINATION
OCULAR EXAMINATION
PHYSICAL EXAMINATIONS
Head
It is assessed for size, shape and position. Large size of head occurs in hydrocephalus. Abnormal head posture occurs in extraocular muscle paralysis as compensatory mechanism to avoid diplopia.
Facial Symmetry
It is looked for abnormalities of facial bones, muscular atrophies and facial nerve paralysis.
Position of Eyeballs
It is looked for the presence of misalignment (squint) and forward displacement of the eyeball (proptosis). Normally, when light is directed to the eyes in midline, symmetrical central corneal reflexes are present, but in squint or the displacement of the eyeball, one or both corneal reflexes will be eccentric (non-central).v
Eyelids
a. Skin
It should be normal on both sides with the presence of upper eyelid crease, which is about 5 mm from the eyelid margin. It is absent in congenital and traumatic ptosis.
b. Lid Margin
Is looked for congestion, swelling, exudate, dandruff or scales, entropion and ectropion.
C. Eye Lashes
c. Normally, two rows of eyelashes are present in each eyelid. Lashes are examined for madarosis, matting of lashes, trichiasis, distichiasis and metaplastic lashes.
Inter Palpebral Fissure Width
This is the space between the two eyelid margins, measured from the center. Normally, it is 9-11 mm and upper eyelid covers 1-2 mm of cornea at 12 o’clock position. The fissure
width may be: Narrow in-
- Ptosis, blepharospasm and photophobia
- Enophthalmos
- Wider in
- Retraction of the upper eyelid Proptosis
Lacrimal System
Consists of
i. Secretory system (lacrimal glands). The increased secretion by glands causes watering called lacrimation. The causes of lacrimation include:
- o Foreign body o Inflammation
- In conjunctiva or cornea
- Conjunctivitis
- Keratitis
- Acute iridocyclitis
- Glaucoma
- Acute congestive glaucoma
ii. Drainage system includes puncti, canaliculi, lacrimal sac and nasolacrimal duct. Obstruction to the drainage system causes watering called ‘Epiphora”. Obstruction to the nasolacrimal duct causes positive regurgitation test.
Method of Regurgitation Test
Ask the patient to look up and press upon the lacrimal sac with little finger or pull the lower eyelid down with middle finger and press upon the lacrimal sac with index finger, the contents of lacrimal sac will come out of puncti
Conjunctiva
Is looked for the presence of redness, congestion, chemosis, discharge (exudate), papillae, follicles, membrane, pseudo membrane, foreign body, symblepharon, and growth. For descriptive purpose, it is divided into palpebral, fornix and bulbar conjunctiva. It is examined by:
a. Eversion of Lower Eyelid
Method: Ask the patient to look upward and pull the lower eyelid in downward direction with index finger, which makes the lower half of the conjunctiva visible
b. Eversion of Upper Eyelid Method:
Ask the patient to look downward, grasp the lashes between the thumb and the index finger, pull the eyelid gently downward (Fig. 4.3 A) and evert it with the tip of index finger, which makes the upper half of the conjunctiva visible.
Limbus (Circumcorneal Region)
This area corresponds to the area between cornea and sclera. It is supplied by the superficial branches of anterior ciliary arteries. Circumcorneal congestion is also called aliary congestion, which is typically found in:
- Keratitis
- Acute congestive glaucoma
- Acute iridocyclitis
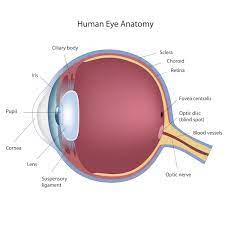
9. Cornea
Shape of the Cornea: Normally it is smooth and convex. Abnormal bulging occurs in keratoconus, megalocornea and congenital glaucoma.
ii. Corneal Diameter:
- o Normocornea
- o Microcornea
- 11 to 12 mm
- 10 mm or less.
- Megalocornea
- 14 mm or more
III. Corneal transparency:
Normally, corneal surface is covered with a tear film. It is bright, lustrous and transparent. Cornea should remain clear for its refractive purpose. Transparency of cornea is lost by oedema, opacity, vascularization, pigmentation, dystrophy and degeneration. The refractive power of cornea is +43 diopters.
iv. Corneal Sensitivity:
Normal, cornea is sensitive to touch. Method to assess corneal sensitivity Ask the patient to look straight ahead and touch the commea with the tip of a cotton swab from temporal side. Patient with the normal corneal sensation will blink relexivel The reduced sensation occurs in:
- o Viral keratitis
- o Corneal dystrophies
- o Lesions at the apex of orbit, involvmglacy nerve.
- Damage to trigeminal ganglion by surgesy or alcohol injection.
- o Cerebellopontine angle tumour (acoustic neuroma).
Corneal staining:
It is done to detect the corneal epithelial defect or ulcer by instillation of vital dyes.
- 2% Fluorescein is an organic dye, which stains the damaged epithelial areas that appear greenish when viewed with blue light.
- 2% Rose Bengal has more affinity for dead and devitalized epithelial cells and mucous. It is useful in dry eyes.
Anterior Chamber
i. Depth:
- Normal is 2 to 3 mm.
- Average is 2.5 mm.
- Shallow, when less than 2 mm e.g. narrow angle glaucoma.
- Deep, when more than 3 mm e.g. aphakia, high myopia and congenital glaucoma.
ii. Flare:
It is the presence of proteins in the anterior chamber. Normally, the beam of light is not visible in anterior chamber but the presence of abnormal proteins reflects the light and makes it visible, e.g. acute iridocyclitis.
iii. Keratic Precipitates (KPS):
These are inflammatory cells deposited on the endothelium of cornea e.g. Iritis and Iridocyclitis
iv. Hypopyon:
It is the presence of pus cells/exudate in anterior chamber e.g. corneal ulcer.
v. Hyphaema:
It is the presence of blood in the anterior chamber e.g. in trauma.
Iris
Iris colour is symmetrical in both eyes. Iris is looked for heterochromia (asymmetry of iris colour), whitish scar, growth, foreign body, neovascularization, anterior synechiae, posterior synechiae, transillumination defect and detachment of iris from its base.
Pupil
i. Shape
- Normally, it is round and regular.
- It is irregular in posterior synechiae, trauma,
- congenital defects and after surgery.
ii. Size
- Normal pupillary diameter is 2-5 mm, and a rage is 3 mm.
- Miotic pupil, when diameter is less than 2 mm.
- Mydriatic pupil, when diameter is more than 5 mm.
iii. Pupillary light reflex (reaction of pupil to light).
Tags: Corneal Sensitivity, History Taking and Examination, III. Corneal transparency:, Inter Palpebral Fissure Width, Lacrimal System, Limbus (Circumcorneal Region), Position of Eyeballs, PROTOCOL OF EYE EXAMINATION, Systemic examination
Top site ,.. amazaing post ! Just keep the work on !